by Leah Alexander
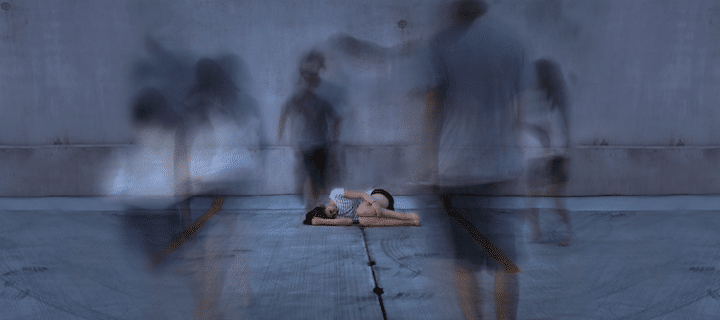
Illustration: “Haunted” by Tatiana Hollander
In any big city, it is fairly common for people to become so accustomed to a busy and competitive lifestyle that they fail to notice the stress that beats through their city like an invisible drum. However, for some—particularly, those who are genetically predisposed to mental health issues—the stress associated with an urban lifestyle is not something that can easily be avoided. Stress hangs over these individuals like a dark cloud, and if they are left in the darkness for too long, the effects of this stress can lead to the unraveling of certain mental health disorders that might have otherwise gone unnoticed. Specifically, individuals residing in urban environments have been found to be significantly more prone to mental health issues, such as mood and anxiety disorders, than those living in more rural environments; in fact, meta-analyses have shown that city dwellers are 21% more likely to develop an anxiety disorder and 39% more likely to develop a mood disorder.1,2 But, perhaps, the most significant—yet, still largely misunderstood and severely stigmatized—of mental health issues to affect those living in cities is schizophrenia, which has an incidence of almost double for city dwellers.2,3
But what are the specific factors of urban environments that could potentially lead to such an abnormally high rate of schizophrenia, as well as other mental health issues, amongst individuals living in cities? One possible explanation could lie in the fact that, with more than half of the world’s population currently residing in cities,2 urban communities are often faced with various issues and constraints as a result of overpopulation and lack of infrastructure. Even in New York City—which is widely viewed as an epicenter of prosperity and wealth—environmental pollution, economic inequality, social exclusion, and other factors particularly associated with urban areas cause many individuals to suffer from stress.4 Cities are also often faced with a lack of green space, in contrast to more rural areas, and this dearth of greenery has been found to negatively affect mental health.5 Access to green zones—such as large, grassy fields or meadows—has been found to alleviate stress through various mechanisms.5 For example, green zones provide ample, natural space for physical activity, which alleviates stress in and of itself.5 Moreover, simply having the ability to directly interact with nature has been found to lower the levels of stress, including the levels of perceived stress, in individuals.5
A pressing question still remains, however: does urban exposure alone lead to the emergence of schizophrenia? A study by Spauwen et al. sought out the answer to that very question and proposed two different models that predicted the effect of urbanicity on levels of psychosis associated with schizophrenia within a group (Fig. 1). Model 1A shows that the effect of urbanicity is only significant once the schizophrenia threshold has been reached.6 This model implies that the psychosis phenotype in individuals exposed to urban environments only appears when combined with another rare cause for schizophrenia, thus suggesting that urban exposure alone does not induce psychosis.6 However, model 1B displays an entire shift in the psychosis distribution. In this model, those exposed to urbanicity show a significantly higher population level of psychosis than those that are non-exposed, suggesting that something in the urban environment enables a shift to higher population expression of psychosis affiliated with schizophrenia.6 Ultimately, this study, which was carried out in a young population growing up in urban and rural environments, produced results that correlated with model 1B: exposed individuals as a group displayed higher levels of schizophrenia-related psychosis than non-exposed individuals, indicating that continuous exposure to city-related stresses during upbringing forms the basis for the association between urbanization and schizophrenia risk.6
Another aspect of urban upbringing believed to be associated with schizophrenia is social stress. For example, schizophrenia incidence amongst the Swedish population was found to be strongly correlated with social fragmentation, a characteristic of urban neighborhoods lacking in social bonding and unity.7,8 This finding is further supported by a study conducted by Lederbogen et al., which found a connection between urban upbringing in healthy adults and elevated neural activity under social stress in the perigenual anterior cingulate cortex (pACC), an area of the brain responsible for stress and regulation of emotions.2 However, in a later study that specifically focused on the differences in gray matter volume in the pACC between males and females who had an urban upbringing, only males were found to have a decrease in gray matter volume as a result of urban upbringing.8 This decrease in gray matter of the pACC found only in males is consistent with previous observations that males—particularly, those that were raised in urban environments—are significantly more prone to developing schizophrenia.8-10
A substantial factor in determining how one is affected by urban social stress that can potentially lead to schizophrenia is his or her unique genetic makeup. Specifically, certain variants in the oxytocin (OXTR) receptor gene, as well as in CACNA1C, a gene encoding the alpha subunit of the L-type voltage-dependent calcium channel, have been found to be linked to social dysfunction responsible for disrupting the coupling of the anterior cingulate cortex (ACC) to the hypothalamus and the amygdala (Fig. 2a).11 Moreover, particular social environmental risk factors for schizophrenia, such as urban upbringing and social status processing, have been found to provoke ACC activation (Fig. 2b).11
Despite these correlations between genetics and social environmental factors that strongly support a causation hypothesis, many still believe in a selection hypothesis: urbanicity does not cause schizophrenia, but, instead, more individuals who are predisposed to schizophrenia move to urban areas.3 This hypothesis, however, appears to be dubious; if genetic risk was the true factor underlying the connection between urban exposure and schizophrenia, then changes in urban exposure during childhood would not alter the risk of schizophrenia later in life, because the true factor of genetic risk would remain unchanged.3 However, as two different studies reveal that early changes in urbanicity exposure lead to increased schizophrenia risk later in adulthood, genetic risk is clearly not the ultimate influence behind the prevalence of schizophrenia in urban environments.3
Ostensibly, there is still much to be discovered regarding the potential correlations between urban environment and the neural genetics underlying schizophrenia, and the implication of future research on these interactions is of extreme importance. For example, with urbanicity proving to be such a significant risk factor for schizophrenia, developing nations that are rapidly urbanizing may face the risk of a rise in schizophrenia.1 Future research also has the power to provide a better understanding of this rather obscure mental illness, thus leading to the potential eradication of this disorder someday. Optimally, an increased understanding of the neural mechanisms underlying schizophrenia will not only give rise to the discovery of a cure for the disease but will also work to derail the stigma affiliated with schizophrenia that afflicts city dwellers suffering from the disorder worldwide.