Jessica Meng
Imagine this: You have Hepatitis C. Caused by the Hepatitis C virus (HCV), Hep C can cause serious liver disease and impair liver function. As people cannot live without the liver (unless you want to get renal dialysis, which still cannot completely filter every waste product the way a fully-functional liver can), Hepatitis C is a very serious condition that requires treatment. A few years ago, the main treatment option would have been to take the ribavirin drug combined with pegylated interferons, a combination with a low 50% cure rate and many symptoms including anemia. However, a new drug named Harvoni has appeared on the market. Since November 14, it has become a very effective drug, with millions of success stories to it. Its main downside, like every new drug, is its “newness.” There is little data collected about its long-term effects. So far it seems to be safe, only causing minor headaches and fatigue. All the same, there is a chance that Harvoni may cause some other health condition further down the road. As the patient, you must choose whether the risks outweigh the benefits. Would you play it safe and take ribavirin-interferon? After all, it is possible that it works and you won’t get anemia. Or would you risk it and take Harvoni, only to find out years later that the drug can cause a serious complication in the future?
Before you make your choice, first understand how Hep C works. HCV is blood-borne, meaning that it can be passed through sexual contact or contact with blood, used needles, people with HIV/ AIDS, men who have sex with men, blood transfusions before 1989, and dialysis equipment that has been improperly sterilized. It can also be hereditarily transferred from mother and/or father to child. Hep C viruses use single-stranded RNA to carry their genetic info (Barnes 2013, Rosen 2011). Due to having RNA instead of double-stranded DNA, these viruses lack polymerase enzymes that can correct any mismatched nucleotides that make up DNA and RNA. Therefore, these viruses are subject to increasingly high rates of mutation (Carroll & Olsen, 2006).
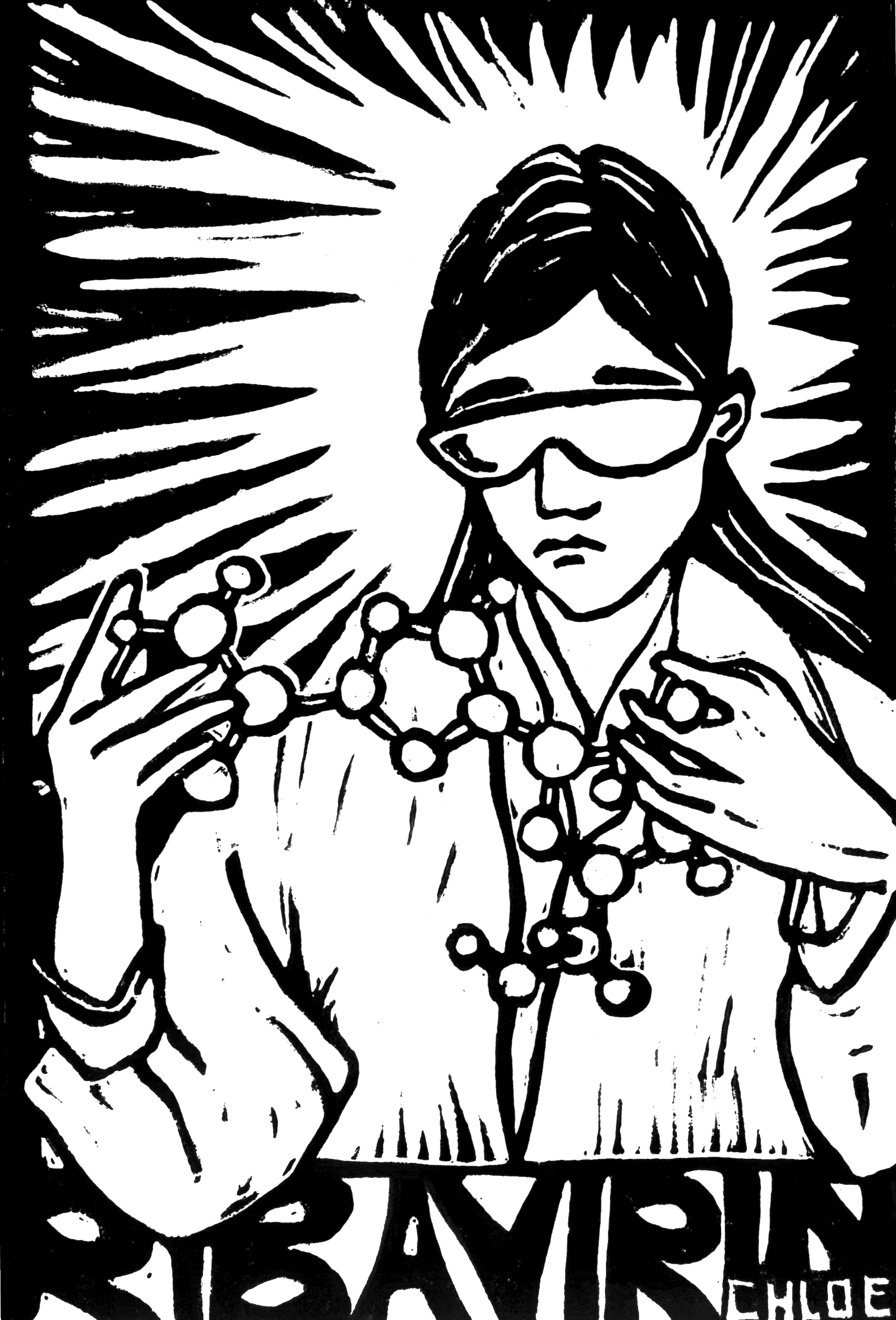
Ribavirin works by capitalizing on this lack of polymerase activity (Barnes 2013, Te Et. Al. 2007). RNA and DNA are both composed of a pentose sugar, nucleobase, and three phosphates, which form what is called the phosphate backbone. The ribavirin molecule is structurally very similar to both RNA and DNA except for an alteration in one of these three components. Additionally, the drug has a carboxamide group (made of carbon, hydrogen, oxygen, and nitrogen) that makes it structurally similar to two nucleosides (Witkowski Et. Al. 1972). Nucleosides themselves are structurally similar to nucleotides except that they have fewer than three phosphate groups. When ribavirin is incorporated into RNA during viral replication, the carboxamide group fools the virus into placing ribavirin where these nucleosides should have been placed. This results in mutations in the RNA and the failure to produce the correct gene products. At a high dose, this technique effectively prevents further replication of the virus and should lead to the patient’s full recovery (Te Et. Al. 2007). This mutation concept behind ribavirin makes it highly effective against a majority of RNA viruses such as those that cause Severe Acute Respiratory Syndrome (SARS), influenza, and hemorrhagic fevers (Tam Et. Al. 2001, Kirk Et. Al. 2009, Rina 2015).
While ribavirin can induce RNA mutations, its effectiveness is enhanced with the addition of pegylated interferons (Hartwell & Shepherd 2009). Interferons are constantly created by the immune system to fight all kinds of viral and bacterial diseases. These highly specific proteins attach to cells to defend healthy ones from invading viruses, to target infected cells for destruction, and to prevent viruses from replicating (National Viral Hepatitis Program 2015). Pegylation refers to the addition of the polyethylene glycol compound (PEG) which, when added, makes the interferon molecules larger. This increase in size keeps the interferons in the blood much longer (Foster 2010, Baker 2003, Cutler 2006, Daniel 2014).
However, there are many issues with this ribavirin-interferon combination. The treatment has a 50% cure rate and has a wide range of symptoms such as fatigue, headaches, irritability, depression, insomnia, diarrhea, and nausea (National Viral Hepatitis Program 2015, Bruchfield Et. Al. 2006). This treatment has also lead to hemolytic anemia in 10% of patients who took it. Hemolytic anemia is a very serious, potentially life-long health condition: it is when red blood cells are destroyed and removed from the blood prematurely. These RBCs are in charge of bringing oxygen throughout the body, so shortages of oxygen can be responsible for many of ribavirin-pegylated interferon’s symptoms like fatigue and headaches (Mura Et. Al. 2004, National Heart, Lung, and Blood Institute 2014). The exact mechanism of how ribavirin leads to anemia is still unknown even after forty years, but there is one popular hypothesis. As HCV affects the blood, ribavirin-pegylated interferon goes into RBCs. There, it is predicted that the drug has phosphate groups added to it through a process called phosphorylation. RBCs do not have enzymes that can remove the phosphate group through the process of dephosphorylation, so this phosphorylated ribavirin can accumulate until it destroys these red blood cells (Carroll & Olsen 2006).
For forty years, a majority of Hep C patients have taken ribavirin-PEG-interferon treatment and put up with all of its symptoms. However, a new medication called Harvoni has been on the drug market since November 2014. Both interferon and ribavirin-free, Harvoni effectively treats patients with Hep C genotype one (the most common version of the disease in the US; there are between six to eleven types in total) (Hirsch 2014). Harvoni contains two antiviral drugs called sofosbuvir and ledipasvir. Sofosbuvir is a HCV polymerase inhibitor, which blocks the enzyme that the virus needs to replicate with. Ledipasvir inhibits a phosphoprotein called NS5a that is involved in viral replication (Fransciscus). Prevented from replicating, the limited quantities of HCV can eventually be fully destroyed by the immune system.
What makes Harvoni better than the ribavirin-interferon combination? Its side effects include mild headaches or pain, nothing compared to ribavirin’s many symptoms. With Harvoni, an outdated form of treatment, but still works—to some extent. However, as more medications like Harvoni no phosphorylation and subsequent dephosphorylation of red blood cells is needed, so no dangerous anemia results (Infohep.org n.d.). Most astonishingly, Harvoni has a whopping 90% cure rate compared to ribavirin-interferon’s 50%. Harvoni is the most effective treatment for Hep C so far. Millions of success stories confirm it (Heitz 2014).
So what about ribavirin? The drug has been on the market since its development in 1970 (Mestrovic 2015). It may be an outdated form of treatment, but still works—to some extent. However, as more medications like Harvoni arise, ribavirin may find itself going out of circulation. Even though its exact mechanism of action is still a mystery, its availability has certainly revolutionized the drug market and cured the illnesses of millions of people in its forty-year run. Though ribavirin has its faults, the drug certainly has helped lead scientists, doctors, and patients one step closer to the complete cure of Hepatitis C.
So, if you are a patient diagnosed with Hep C within the past year, you’re one of the
lucky ones who can have access to an anemia-free treatment. Harvoni so far proves to be a very good drug, although it is fairly new. As the patient, it is ultimately your choice whether you’d want to go with ribavirin-PEG-interferon, whose effects are known, or with Harvoni, whose long-term effects have yet to be fully discovered.